The anal canal is the last part of the rectum before the anus. When the lining of the anal canal develops a tear or a sore (ulcer), it is called an anal fissure. Fissures can occur in anyone but are more common in middle-aged or young adults. A fissure can be difficult to heal as it causes a spasm in the anal sphincter and aggravates itself, creating a vicious circle of pain and irritation.
Symptoms Of An Anal Fissure
Symptoms of a fissure include :
Bright red blood in the toilet bowel or on paper.
Painful bowel movements.
Diagnosing Anal Fissures
A fissure is typically diagnosed via either a visual or a digital rectal exam. A special tool called an anoscope or a sigmoidoscope may also be used. Either of these two tests can determine if any bleeding from the anus is truly from a fissure or caused by a different problem.
Causes Of An Anal Fissure :
Fissures can be caused by constipation or by forcing a hard bowel movement through the anus, during childbirth, or ulceration of hemorrhoids.
There are several risk factors for fissures. These include:
Anal sex
Constipation
Crohn’s disease
Chronic use of laxatives
Immunodeficiency disorders
Leukemia
Multiple pregnancies
Treating Anal Fissures
Fissures are treated in a variety of ways. A physician will help you understand the treatments, their differences, and which one is most appropriate for you.
Acute Fissures. For acute fissures, treatment aims to lessen pressure on the anal canal by making sure stools are soft and to ease any discomfort or rectal bleeding. These methods include:
Warm baths (or Sitz baths)
Eating more fiber to create softer stools
Stool softeners (as prescribed by a physician)
Topical hydrocortisone (suppositories or foams)
Zinc oxide
Petroleum jelly
Topical anesthetics for pain
Topical nitroglycerin cream
Patients may also be advised to avoid straining during a bowel movement, and to drink at least 8 glasses of water per day to prevent constipation. Cleaning the anal area with warm water after bowel movements may also be recommended. About 90% of fissures will heal without surgery.
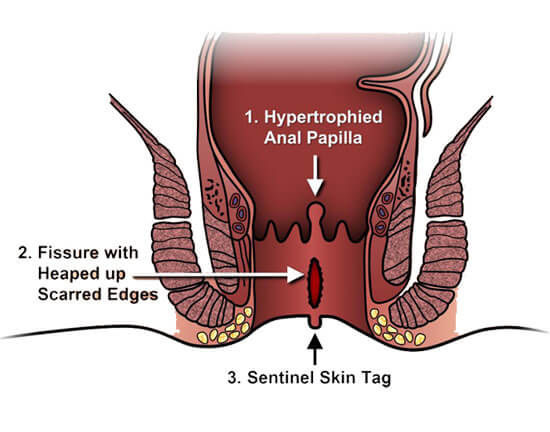
Chronic Fissures: If a fissure persists even after treatment, it may become chronic. A chronic fissure may need to be treated with surgery. Two types of surgery are done for fissures — anal dilation and lateral internal sphincterotomy (LIS). Anal dilatation may be a choice for some patients, but it is being used less often due to the potential of incontinence as a complication. During anal dilatation, the anal canal is stretched. More often, the LIS surgery is used. LIS is usually done with a general anesthetic on an outpatient basis. In the procedure, a portion of the anal canal muscle is cut. The fissure itself is not removed, but any muscle spasms in the anus sphincter will be relieved. This will allow the fissure to heal at a cure rate of more than 90%.
After surgery, it is important to keep the anal area clean and dry. Moist wipes instead of toilet paper and a stool bulking agent may be recommended.
Newer Treatments
One new non-surgical method being researched for use in healing fissures is Botox (botulism toxin) injections. The injections work by weakening the anal muscles and thereby allow them to heal. This method is considered more invasive than other non-surgical options, but it has a higher success rate than treatment with nitroglycerin.
How Fissures Relate To Other Conditions
Fissures are more common in people with Crohn’s disease than in those who have ulcerative colitis. Elderly people or those who have diabetes may have more difficulty in healing fissures. Fissures are not related to colon cancer.
The Prognosis For Fissures
The prognosis is good for acute fissures; they generally heal with non-invasive treatments. The cure rate using LIS surgery for chronic fissures is also encouraging. LIS can be repeated if the fissure does not heal with the first surgery. Fissures do not cause cancer and complications are uncommon.
If you are suffering from Fissure and want safe, effective treatment, do contact us.
